




by Dr. Hy Gia Park and Dr. Charles Park
“Can’t you just be happy?! Get over it! It’s only in your head.”
These are typical remarks that depressed individuals frequently hear. Implicit in these statements are: if you are depressed, you are not trying and feeling happy means you are better. These are all misconceptions and it is time to set the facts straight about clinical depression.
Emotions like happy and scared are sensory data about intrapsychic states resulting from interactions with others and the environment and should be used for navigating life, not goals for depression treatment. Rather than “being happy,” achieving remission from depression means stabilizing cognitive function so that the individual can once again, engage in meaningful relationships and hobbies, and feel a sense of life purpose. Individuals suffering from this medical condition need to be able to understand how to use these data sets to increase their capacity to love, play, and work, and this in turn, leads to the commonly desired treatment goals of happiness and contentment. Emotions provide the guidance needed to make ‘right’ choices and decisions throughout life; they are often the ‘fuel’ or “gut feelings” that impel us to act or not. They guide and organize a group of brain functions called executive functioning that allow humans to plan, problem solve, execute, and arguably the most important function, suppress impulsive and/or counter-productive behaviors that may interfere with achieving life goals. Many of these cognitive activities are regulated by the front part of the brain, the prefrontal cortex (PFC). The PFC is in constant back and forth communication with, regulates (as well as being regulated by) more ‘reptilian’ automatic parts of our brain, where the fight-or-flight survival response resides. Ironically, depression, may actually arise from this stress system working a little TOO well.
Depression affects 7.1% of adults in the United States and studies suggest that this is the same rate, if not higher in athletes.1
Theories about depression have evolved beyond serotonin levels. Newer theories suggest that depression is actually a survival response (albeit prolonged) arising from long-term exposure to stress(es).2 Before continuing this discussion of depression, we do need to agree on definition of certain terms. Homeostasis is defined as the body’s baseline chemical state that it fights to maintain. Stress can be defined as any internal and external stimuli that disrupt homoeostasis. When the brain’s homeostasis is challenged by stress be it internal (e.g. “will I make the team?”), interpersonal stress (e.g. relationships with coaches and teammates), chemical (e.g. drugs or alcohol) or environmental (e.g. playing on turf versus grass), this stress leads to a cascade release of certain brain chemicals.
Stable brain chemistry is required for the brain to function properly and minimize the symptoms of depression. For the purpose of this discussion, a normal homeostatic brain is akin to a heating/cooling system where the thermostat is set at a comfortable 68° F. Any form of stress will initially and temporarily push the thermostat or neurochemistry of the brain (e.g. serotonin, dopamine levels) out of whack. The programming of the brain has evolved over time to always maintain the thermostat setting at 68° F so it immediately responds to the change by releasing a series of chemicals to bring the thermostat setting back to normal. Stress chemicals such as, glutamate, norepinephrine, cortisol, and corticotropin releasing factor lead to either over-functioning or under-functioning of neurocircuits to illicit a rapid response to danger. Turning off PFC function and allowing more automated, primitive parts of the brain to respond to danger is more efficient. The problem in depression is that the brain is stuck in this mode even if we have successfully averted danger but now, the new thermostat setting has been re-set to 80° F, regardless of appropriateness. Prolonged over/under-functioning in these neurocircuits in response to this new thermostat setting causes the body’s fight-or-flight system to stay on longer than necessary and leads to dysfunction of thinking and behaviors, the phenomenon we call clinical depression.
Disability from depression comes from the body’s response to prolonged stress, which ultimately atrophies the PFC. This explains why depression is the fourth leading cause of disability worldwide and current epidemiological trends project that by 2020 it will become the second leading cause of disability worldwide.1 Individuals with depression lose their ability to correctly and rationally interpret and respond to sensory data. They will often say they are not sad but describe difficulty engaging in pleasurable activities – “I just work and sleep.” A sense of worthless or guilt completely out of proportion to the perceived sin is common and ultimately leads to the internal experience of hopelessness. Excessive fatigue, fogginess of memory and thinking, low motivation, appetite changes, sleep problems, poor concentration make the simplest of tasks appear overwhelmingly challenging. Effective depression treatment should address both the disruptions in the neuro-chemicals and the neuro-circuits.
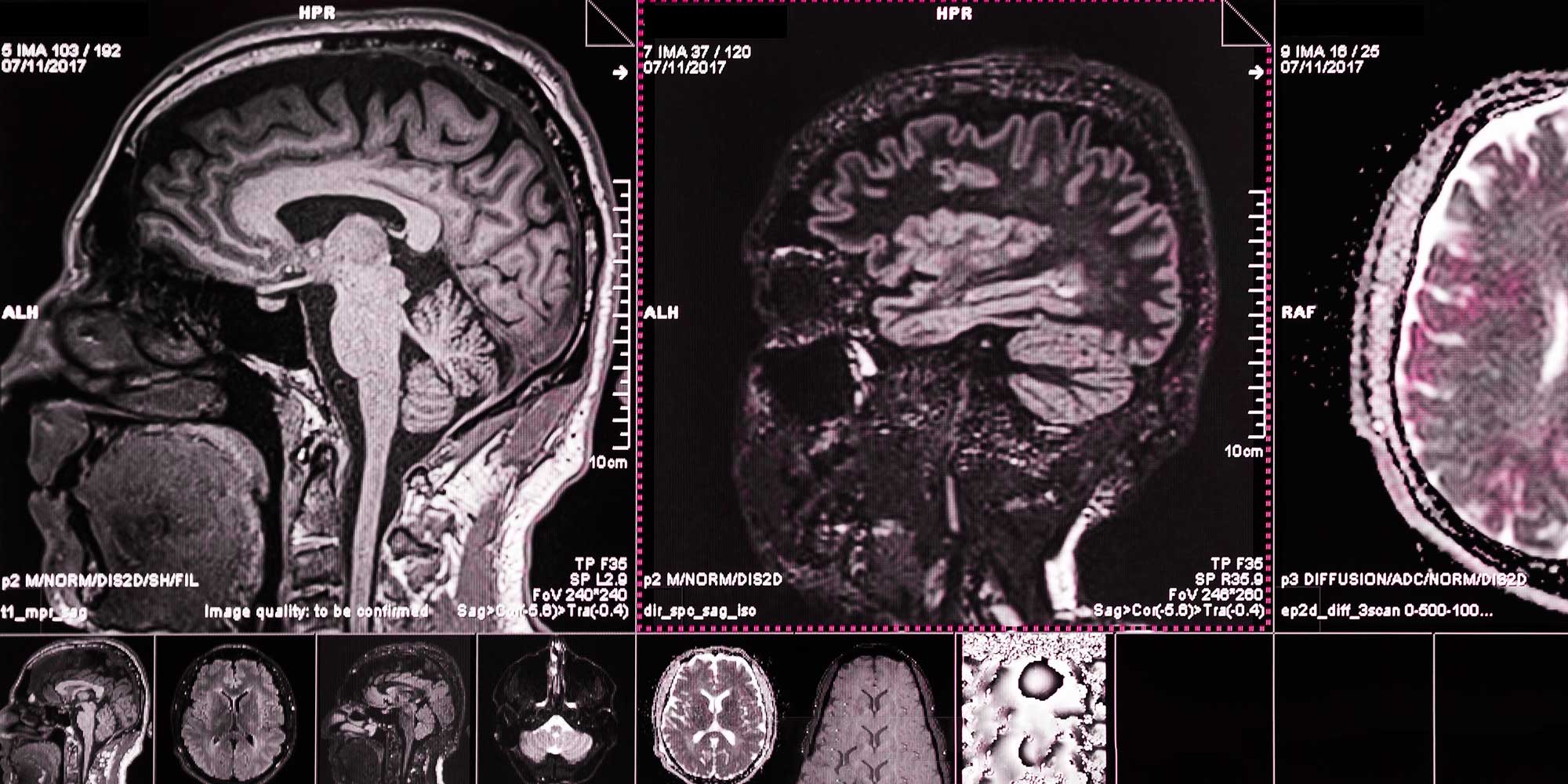
Up until the last decade, the options for depression treatment have been limited to medications to treat the neurochemical disruptions and psychotherapy to address the dysfunction in the neurocircuits. Enter Deep Transcranial Magnetic Stimulation (dTMS), a novel medical procedure similar to Magnetic Resonance Imaging (MRI). It is an emerging non-invasive brain stimulation technique that uses magnetic fields to stimulate brain cells without the need for medications or anesthesia. With dTMS, an electromagnetic coil placed adjacent to the scalp is used to apply brief magnetic pulses to the brain. The painless magnetic pulses modulate brain network activity in the region of your brain involved in mood regulation, depression, and anxiety. It’s like physical therapy for sports injuries. Focal targeting of the specific brain regions believed to be involved in depression leads to quicker improvements while avoiding systemic side effects common with antidepressant medications, such as fatigue, upset stomach, weight gain, and sexual dysfunction. Clinical studies have demonstrated dTMS’s effectiveness in normalizing PFC brain circuits and its general tolerability, which can be a game changer for the estimated 17.3 million adults in the United States who suffer from depression.3
At the end of the day, clinical depression is better seen from its cognitive dysfunction than whether or not the individual is “happy or sad.” It is the cognitive dysfunction that causes disability and hurts the individual and their loved ones. Furthermore, the irrationality that reflects the cognitive dysfunction is what creates the profound pain experienced with this illness. From the less extreme irrationality seen in the expressed thoughts and feelings of worthlessness, to the more concerning expressions of feeling trapped or hopeless, rapid treatment is necessary as the most profound expression of irrational hopelessness can be seen in the disease’s most dangerous symptom: thoughts and actions related to suicide.
Sources